2. Classes of antidepressant drugs
- Tricyclic and related antidepressant drugs
- MonoamineOxidase Inhibitirs (MAOIs)
- Selective Serotinin Reuptake Inhibitors (SSRIs)
- Other antidepressant drugs.
3. Mechanisms of actions of antidepressants
4. Common side effects of antidepressants
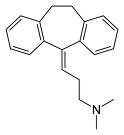
5. Tricyclic and related antidepressant drugs
- Amitriptyline Hydrochloride
- Amoxapine
- Clomipramine Hydrochloride
- Dosulepin Hydrochloride
- Doxepin
- Imipramine Hydrochloride
- Lofepramine
- Nortriprtyline
- Trimipramine
6. Monoamine Oxidase Inhibitors
- Phenelzine
- Isocarboxazid
- Tranylcypromine
- Moclobemide
7. Selective Serotonin Reuptake Inhibitors
- Citalopram
- Escitalopram
- Fluoxetin
- Fluvoxamine maleate
- Paroxetine
- Sertraline
8. Other antidepressant drugs
- Flupentixol
- Mirtazapine
- Reboxetine
- Tryptophan
- Venlaflaxine
9. Drug interactions
- Drugs interactions with Tricyclic and related antidepressant drugs
- Drugs interactions with MonoamineOxidase Inhibitirs (MAOIs)
- Drugs interactions with Selective Serotinin Reuptake Inhibitors (SSRIs)
- Drugs interactions with other antidepressant drugs.
10. New developments